September/October 2021
Managing Dysphagia — The Importance of Safety, Variety, and Training A diagnosis of dysphagia is a stressful. Not only is the swallowing disorder physically taxing on patients but it’s also psychologically, emotionally, and socially demanding for patients and members of their care teams—especially at mealtime. Food and drink can elicit many emotions—comfort, joy, and nostalgia, to name a few. Furthermore, mealtime allows individuals to connect with their loved ones and culture and influence their health multiple times a day. For those with dysphagia, however, mealtime can bring fear, embarrassment, and isolation. Each swallow poses a risk of choking or aspirating—breathing in foreign material such as food, drinks, and saliva—and with each meal, health care professionals and caregivers often worry whether they’ve prepared the food or beverage to the appropriate consistency. The good news is there are several ways to mitigate this risk and help patients manage their swallowing disorders, encourage dining with dignity, and improve quality of life. When it comes to dysphagia and modified diets, health care professionals should prioritize safety, variety, and comprehensive team training. Promoting Patient Safety via IDDSI One of the main ways to promote safe swallowing and better airway protection for patients with dysphagia is via a diet of modified food textures and thickened liquids. Texture-modified diets have long been recommended by practitioners for dysphagia patients; however, there’s a new standard of practice being implemented worldwide: the International Dysphagia Diet Standardisation Initiative (IDDSI). In fact, the American Speech-Language-Hearing Association supports the IDDSI framework, and the Academy of Nutrition and Dietetics recently announced that it will no longer support the previously used National Dysphagia Diet and instead will include only IDDSI in its Nutrition Care Manual beginning October 2021. IDDSI Framework and Testing Methods
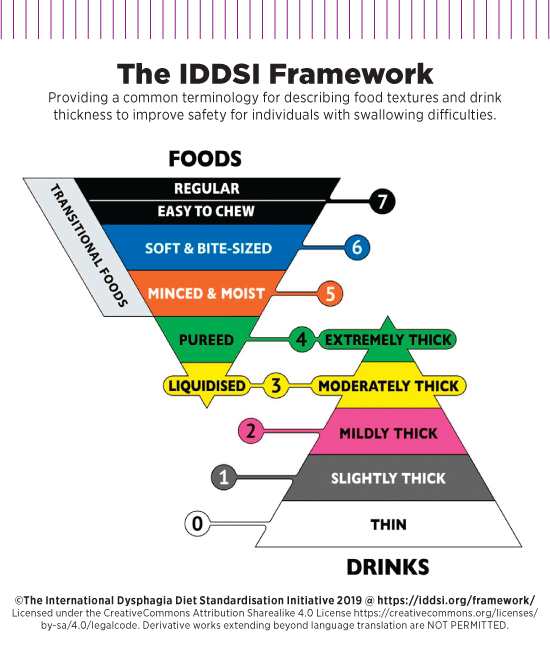
The IDDSI framework consists of a continuum of eight levels (0 to 7); drinks are measured from levels 0 to 4 and foods are measured from levels 3 to 7. The framework promotes patient safety through standardized language across all age groups and care settings; each level is linked with a specific name, color, and number. The top section of the IDDSI framework focuses on foods, with the following levels represented by the triangle with the tip pointed down: • Level 3: Liquidized—Can be drunk from a cup or eaten with a spoon, has a smooth texture with no “bits,” and can be swallowed directly (no oral processing or chewing is required). • Level 4: Puréed—Usually eaten with a spoon, does not require chewing, and cannot be poured, drunk from a cup, or sucked through a straw because it does not flow easily. • Level 5: Minced and Moist—Soft, moist, and minced with no separate thin liquid, can be eaten with a fork or spoon, and small lumps visible within the food are easy to squash with tongue. • Level 6: Soft and Bite-Sized—Soft, tender, and moist throughout and bite-sized with no separate thin liquid. Can be eaten with a fork, spoon, or chopsticks and chewing is required before swallowing. • Level 7: Easy to Chew—Normal, everyday foods of soft/tender textures that are developmentally and age appropriate and can be eaten via any method. • Level 7: Regular—Normal, everyday foods of various textures (may be hard and crunchy or naturally soft) that are developmentally and age appropriate and can be eaten via any method. The bottom section of the framework concerns drinks, with the following levels represented by a triangle with the tip pointing up: • Level 0: Thin—Flows like water and can be drunk through any type of teat/nipple, cup, or straw as appropriate for age and skills. • Level 1: Slightly Thick—Thicker than water, requires a little more effort to drink than thin liquids, and flows through a straw, syringe, or teat/nipple. • Level 2: Mildly Thick—Flows off a spoon, and mild effort is required to drink this thickness through a standard bore straw. • Level 3: Moderately Thick—Can be drunk from a cup or eaten with a spoon, has a smooth texture with no “bits,” and can be swallowed directly (no oral processing or chewing is required). • Level 4: Extremely Thick—Usually eaten with a spoon, does not require chewing, and cannot be poured, drunk from a cup, or sucked through a straw because it does not flow easily. It’s important to note that on the framework, Level 3 (liquidized foods and moderately thick drinks) and Level 4 (puréed foods and extremely thick drinks) are connected. This is because foods and drinks at these levels have a similar flow, textural characteristics, and descriptions. In addition to standardizing the language and definitions for each level, which in itself improves patient safety, IDDSI has introduced easy and accessible testing methods to ensure accurate food and drink preparation. These testing methods empower all who prepare foods, serve foods, or assist with meals to easily and quickly test to make sure that patients are getting the food textures and thickened liquids as prescribed. IDDSI testing is done with simple tools such as a 10-mL syringe for testing thickened liquids and a spoon and a fork for testing foods. According to IDDSI, using these common eating utensils—which are inexpensive and available in most food preparation and dining environments—helps minimize the need for subjectivity that often accompanies description-based methods. A welcome outcome of IDDSI testing is that along with safety, food quality improves because there’s a greater focus on the foods and drinks served. When evaluating drinks and liquidized foods, practitioners should use the IDDSI Flow Test, which utilizes a 10-mL syringe as a simple, practical objective measure to classify drinks based on their rate of flow. When testing texture-modified foods, practitioners should use the Fork Drip Test, Spoon Tilt Test, or the Fork or Spoon Pressure Test (a combination of tests may be required). Demonstrations of these tests can be found at IDDSI.org. One of the easiest ways to ensure safety through IDDSI is to use commercially available prethickened beverages that meet IDDSI standards. This takes the guesswork and risk out of hand-mixing—which is more costly and labor intensive, requires additional training, and may pose a choking risk for patients if the beverage isn’t thickened appropriately. This also frees up the kitchen staff to focus on preparing the food to the appropriate consistency. IDDSI will continue to have a meaningful influence on the safety and quality of texture-modified foods and thickened liquids served to those with dysphagia, as errors made in the preparation of a dysphagia diet can lead to numerous and serious adverse health events, such as choking or aspiration. In fact, people older than 65 years of age have seven times higher risk for choking on food than do children aged 1 to 4 years, and for patients with dysphagia, the risk is even higher. Furthermore, approximately one-half of people with dysphagia experience aspiration, which can lead to aspiration pneumonia, a serious and sometimes fatal condition. In addition to following the IDDSI framework, there are several ways to promote safe swallowing via the dining environment itself, such as the following: • Allow the patient to rest for 30 minutes prior to mealtime to ensure they are refreshed and alert, and create a quiet, well-lit, comfortable atmosphere. Safely enjoying their food and drink should be the main focus; limit distractions as much as possible. • During mealtime, sit the person upright in a chair and ensure both the table and chair are at an appropriate, comfortable height. If the individual is confined to a bed, elevate the backrest to a 90-degree angle. • Eating quickly increases aspiration risk. Allow the patient plenty of time to enjoy the meal and the company. • Ensure necessary assistive devices such as adaptive utensils and dishware are ready and available. • Make sure the patient’s mouth is clear before offering more food or drink, alternate solid and liquid boluses, and vary the placement of food in the person’s mouth according to the type of swallowing disorder or other deficit the patient has. For example, if the patient has facial weakness on the right side, food may be placed on the left side of the mouth. • Help patients maintain good oral hygiene throughout the day, including proper teeth brushing and well-fitted dentures, if required. Offering Variety and Encouraging Dining With Dignity While living with dysphagia is difficult, it can be managed with a good care team and proper procedures. Health care professionals working with dysphagia patients should first and foremost educate patients and their caregivers on the need for and benefits of a texture-modified diet and/or thickened drinks. Additionally, helping instill within the patient a feeling of safety and self-directed care can promote confidence and help patients dine with dignity. There are a number of ways geriatric professionals can support those with dysphagia, including the following: • If patients are able, encourage them to dine with friends, family, and other clients. Older adults report feeling happier eating with others, and more than one-half say sharing a meal makes the food taste better. • Serve patients the same foods others are eating, modified for their swallowing abilities, and use molds and pastry bags to make food look appetizing. Many patients—understandably so—don’t want to drink a product that looks medicinal or eat something that looks like baby food. • Nutrient density is key, so it’s important to make every spoonful count. Start with the same delicious and nutritious food being served to other patients and modify it with food and beverage thickener using standardized recipes to achieve the appropriate consistency for each patient. The food and beverage thickener is key, as it will help stabilize the food and retain its form and texture to help lessen the patients’ choking risk. • Communicate with patients and their caregivers. Let the patients weigh in on their preferences for what, where, and how they eat. Taking the time to understand patients’ likes and dislikes will help providers better customize a modified diet for them and ultimately make mealtime more enjoyable. • Offer familiar comfort foods. For example, when ground or puréed appropriately, a meal consisting of meatloaf, mashed potatoes, and carrots will taste and smell like what the patient is used to tasting and smelling prior to their dysphagia diagnosis. • Plan ahead. Always prepare meals and beverages in the kitchen (rather than tableside) and present it to patients with dysphagia just as you would to anyone else. This helps avoid drawing unnecessary and unwanted attention to those with swallowing difficulties. • Get creative in the kitchen and find new ways to encourage consumption and improve hydration and nutrition. For example, try mixing prethickened ready-to-drink juices into fun mocktails. • Help the patient maintain their dignity with a discreet, adult clothing protector rather than a bib, which can appear juvenile. Additionally, if the individual requires support or assistance while eating, sit at the table with them rather than standing over them, which can feel demeaning. • Continue learning and exploring professional resources for best practices. Elder care professionals have an important opportunity to educate patients and caregivers and help them confidently take their seat at the table. Implementing IDDSI in Health Care Settings Characteristics of a successful IDDSI training program include the following: • a thorough, clear, and organized presentation of information that completely covers the characteristics and testing methods of each IDDSI level; • a focus only on the knowledge and skills the health care team needs to safely and effectively perform their jobs on a daily basis; • multiple formats for presenting materials, including visual representations of IDDSI standards, written word, and opportunities for hands-on testing practice. This helps ensure the training appeals to multiple types of learners, including nonnative English speakers and those who have lower literacy levels; • an emphasis on independent problem solving. After the IDDSI training program, each team member should be prepared to use the testing methods on their own to identify when foods and drinks do or do not meet IDDSI standards; and • messages reinforcing a culture of safety. Still not sure where to begin with IDDSI implementation? The best way to develop an understanding of IDDSI is by learning the standards for one diet at a time, beginning with Puréed (Level 4). Most health care professionals in the dysphagia space are already making purées for patients and therefore have the baseline knowledge needed to start implementing IDDSI; it is only a matter of evaluating purées and adjusting them to meet IDDSI standards. Here’s what practitioners need to know in order to understand Puréed (Level 4): • foundations of Puréed (Level 4); Starting here simplifies the intricate process of implementing IDDSI in an organization. Most important, the team will be familiar with basic IDDSI concepts such as standardized identification of the diet (diet name, color, and abbreviation) and testing—all of which are available at IDDSI.org. Living with dysphagia and caring for those with swallowing disorders brings unique, daily challenges. By implementing these suggestions of promoting a culture of safety within your organization; offering a variety of delicious, nutritious, and flavorful foods and beverages; and developing a comprehensive IDDSI training program, health care professionals will be on their way to helping improve quality of life for patients and caregivers. — Margaret Roche, MS, RD, CSG, CDCES, FAND, is the founder of Roche Dietitians and a nationally recognized leader in nutrition for health care. A champion for nutrition for older adults, she advocates for quality improvement with texture-modified diets. Roche has trained thousands on IDDSI implementation. Her opinions and advice are her own. Roche Dietitians has previously been compensated by Kent Precision Foods Group, Inc, producers of the Thick-It brand family of products, for their research and industry insights. — Susan Norris, MA, is a regional sales manager for the Personal Nutrition Solutions (PNS) division of Kent Precision Foods Group, Inc (KPFG). Under the PNS division, KPFG produces the Thick-It brand family of products, which offers mealtime solutions to help improve quality of life for people with dysphagia as well as the health care professionals and loved ones caring for them. Thick-It is a gold sponsor of IDDSI. |